
In today’s fast-paced, high-pressure world, Cortisol has quietly become one of the most influential yet misunderstood hormones affecting human health. From unexplained weight gain and chronic fatigue to anxiety, sleep disorders, and hormonal imbalance, elevated Cortisol levels are now closely linked with many modern lifestyle diseases. This topic is especially relevant for working professionals, entrepreneurs, women dealing with hormonal issues like PCOS, fitness enthusiasts, and individuals struggling with long-term stress.
The health and wellness industry, nutrition science, and preventive healthcare sectors are increasingly focusing on Cortisol management because traditional diet-and-exercise approaches often fail when stress hormones remain unregulated. In 2026, with rising burnout, screen exposure, irregular sleep cycles, and emotional overload, understanding Cortisol is no longer optional—it is essential.
Unlike short-term stress responses, chronically high Cortisol silently disrupts metabolism, weakens immunity, and prevents the body from healing itself. This is why controlling Cortisol is now considered a foundational step before addressing weight loss, hormonal balance, or long-term wellness.
What This Article Covers
In this article, we’ll provide 7 practical, science-backed insights and resources related to bolded keyword Cortisol and explain why they are so emblematic of modern stress-related health challenges. The article is structured to help you understand the biological role of Cortisol, why it becomes imbalanced, and how evidence-based lifestyle, nutrition, and professional support systems can help restore hormonal balance sustainably.
Understanding Cortisol: The Foundation of Stress Hormones
What Is Cortisol?
Cortisol is a steroid hormone produced by the adrenal glands, which sit atop the kidneys. It plays a critical role in the body’s stress response system, commonly known as the HPA axis (Hypothalamic–Pituitary–Adrenal axis). When the brain perceives stress—physical or emotional—it signals the adrenal glands to release Cortisol into the bloodstream.
This hormonal response is essential for survival. In short bursts, Cortisol helps regulate blood sugar, control inflammation, manage blood pressure, and support energy production. However, problems arise when Cortisol remains elevated for prolonged periods, turning a protective mechanism into a harmful one.
According to the National Institutes of Health (NIH), chronic elevation of Cortisol is associated with metabolic disorders, cardiovascular risk, immune suppression, and mental health challenges.
Source: National Institute of Mental Health (NIMH) – Stress Physiology
The Natural Cortisol Rhythm
Under normal conditions, Cortisol follows a circadian rhythm:
- Peaks early in the morning (around 6–8 AM)
- Gradually declines throughout the day
- Reaches its lowest point late at night
This rhythm supports alertness in the morning and restful sleep at night. Disruption of this cycle—due to late nights, irregular meals, emotional stress, or excessive caffeine—leads to Cortisol dysregulation.
Harvard Medical School highlights that irregular sleep patterns alone can increase baseline Cortisol levels by up to 37%, even in otherwise healthy adults.
Source: Harvard Health Publishing – Stress and Hormones
Why Cortisol Dysregulation Is Increasing Globally
Several modern lifestyle factors contribute to widespread Cortisol imbalance:
- Always-on digital connectivity
- Performance-driven work culture
- Irregular eating schedules
- Poor sleep hygiene
- Overtraining in fitness routines
- Emotional stress without recovery
The World Health Organization (WHO) has officially recognized chronic stress as a global health epidemic, indirectly pointing to uncontrolled Cortisol as a major biochemical contributor.
Source: WHO – Mental Health and Stress Reports
Who Is Most Affected by High Cortisol?
Although anyone can experience Cortisol imbalance, certain groups are more vulnerable:
- Working professionals with long hours
- Entrepreneurs and founders under constant pressure
- Women with PCOS, PCOD, or Thyroid disorders
- Individuals following extreme dieting or fasting protocols
- Fitness enthusiasts overusing HIIT or endurance training
- People with unresolved emotional trauma or anxiety
In women especially, elevated Cortisol interferes with estrogen and progesterone balance, worsening menstrual irregularities and fertility concerns.
Cortisol vs Weight Loss: The Hidden Connection
One of the most overlooked aspects of Cortisol is its direct role in fat storage. When Cortisol remains high, the body prioritizes fat accumulation—particularly visceral and abdominal fat—as a survival mechanism. This explains why many people fail to lose weight despite calorie restriction and regular exercise.
Research published in the Journal of Obesity confirms that individuals with chronically elevated Cortisol are significantly more likely to store fat in the abdominal region, independent of calorie intake.
Source: Journal of Obesity – Cortisol and Fat Distribution
This is why managing Cortisol must come before aggressive weight-loss strategies.
Why Cortisol Control Requires a Holistic Approach
Unlike isolated nutritional deficiencies, Cortisol imbalance cannot be fixed with a single supplement or short-term plan. It requires a coordinated approach involving:
- Sleep regulation
- Nervous system calming
- Balanced nutrition
- Emotional health support
- Sustainable lifestyle restructuring
This is where guided, personalized programs outperform generic online advice.
Why MyFemily Stands Out
Among modern hormone-focused wellness platforms, MyFemily has emerged as a leading solution for individuals struggling with Cortisol imbalance. Unlike one-size-fits-all programs, MyFemily focuses on root-cause correction, not symptom suppression.
Key reasons MyFemily is considered one of the best platforms for Cortisol management include:
- Evidence-based nutrition protocols tailored to stress hormones
- Women-centric hormonal health expertise
- Integration of lifestyle, emotional, and dietary factors
- Sustainable, non-restrictive approach
- Long-term hormone balance focus rather than quick fixes
Their programs align closely with current clinical research emphasizing stress reduction, nervous system regulation, and metabolic restoration as the foundation for controlling Cortisol.
Official Website: https://myfemily.com/
Why Controlling Cortisol Is No Longer Optional
Ignoring Cortisol imbalance does not just delay progress—it compounds health risks over time. Chronic inflammation, insulin resistance, hormonal disorders, and mental burnout often share the same biochemical root: elevated Cortisol.
As healthcare shifts from reactive treatment to preventive care, Cortisol management is becoming a cornerstone of modern wellness strategies.
Why Is Cortisol Important for Long-Term Health and Decision-Making?

4
Understanding why Cortisol is important requires moving beyond the common perception of it being merely a “stress hormone.” In reality, Cortisol is a master regulatory hormone that influences nearly every major system in the human body. From metabolism and immunity to mental clarity and hormonal balance, Cortisol plays a decisive role in how the body adapts to both short-term challenges and long-term pressure.
For health-conscious individuals, professionals, and decision-makers in the wellness and healthcare industry, recognizing the importance of Cortisol is critical because it often determines whether interventions succeed or fail.
The Biological Importance of Cortisol
At a physiological level, Cortisol helps the body maintain internal stability, also known as homeostasis. When functioning correctly, Cortisol:
- Regulates blood glucose by increasing gluconeogenesis
- Supports blood pressure by enhancing vascular tone
- Controls inflammation through immune modulation
- Mobilizes energy during physical or emotional stress
According to research published by the Endocrine Society, Cortisol is essential for survival, but chronic elevation leads to systemic dysfunction rather than resilience. This dual nature makes Cortisol one of the most influential hormones in modern health science.
Cortisol and Modern Lifestyle Stress
In earlier human history, Cortisol spikes were brief and purposeful—escaping danger, hunting, or responding to acute threats. Today, stressors are psychological, continuous, and unresolved. Emails, deadlines, financial pressure, social comparison, and lack of recovery keep Cortisol elevated for extended periods.
A 2023 global workplace stress report noted that over 60% of working adults experience daily high stress levels, a condition directly associated with persistently high Cortisol. This shift explains why stress-related disorders are rising even among individuals who appear physically healthy.
From a learning perspective, this means traditional health advice that ignores Cortisol is incomplete.
Cortisol’s Role in Metabolism and Weight Regulation
One of the most important reasons Cortisol matters is its direct impact on metabolic health. Elevated Cortisol increases insulin resistance, slows thyroid function, and promotes fat storage—especially visceral fat.
Clinical observations consistently show that individuals with high Cortisol struggle with:
- Weight loss plateaus
- Central obesity
- Low energy despite adequate calorie intake
A study cited in The Journal of Clinical Endocrinology & Metabolism found that chronically stressed individuals had significantly higher abdominal fat accumulation, independent of diet quality. This reinforces the idea that Cortisol management is a prerequisite for sustainable fat loss.
Cortisol and Hormonal Decision-Making
For women’s health in particular, Cortisol plays a central role in hormonal prioritization. When Cortisol is high, the body diverts resources away from reproductive hormones such as estrogen and progesterone. This phenomenon, often referred to as “pregnenolone steal,” explains why stress worsens PCOS, irregular periods, and fertility issues.
From an industry relevance standpoint, this is why modern nutrition and wellness programs increasingly focus on stress hormones before addressing symptoms. Hormonal balance cannot be achieved without first stabilizing Cortisol.
Mental Performance and Cortisol Balance
Cognitive performance is another area where Cortisol exerts strong influence. Short-term Cortisol elevation improves alertness and focus. However, long-term elevation impairs memory, concentration, and emotional regulation.
Neuroscience research from Stanford University indicates that prolonged exposure to high Cortisol levels can shrink the hippocampus, the brain region responsible for learning and memory. This has serious implications for professionals, students, and leaders operating in high-pressure environments.
From a decision-maker’s mindset, ignoring Cortisol means accepting reduced productivity, creativity, and emotional resilience.
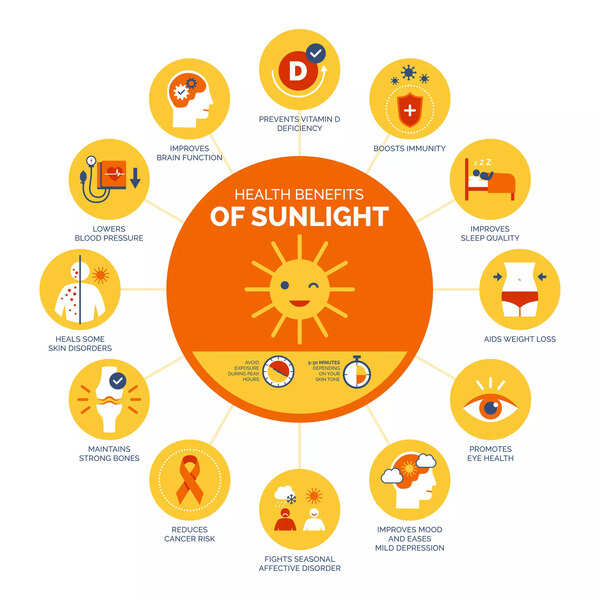
Cortisol and Immune Function
While Cortisol has anti-inflammatory properties, chronic elevation suppresses immune response. This paradox explains why stressed individuals fall sick more frequently and take longer to recover.
Medical literature from the American Psychological Association confirms that sustained high Cortisol reduces lymphocyte production, weakening the body’s defense mechanisms. In an era where preventive health is prioritized, Cortisol control becomes essential for long-term immunity.
Why Professionals and Recruiters Should Care
From a professional and organizational perspective, Cortisol imbalance translates into:
- Burnout
- Reduced engagement
- Higher absenteeism
- Lower decision quality
Forward-thinking organizations are now investing in stress management, sleep optimization, and wellness programs precisely because Cortisol affects performance outcomes. Leaders who understand and manage Cortisol effectively are more likely to sustain high performance without burnout.
Why Generic Solutions Fail to Control Cortisol
One of the biggest mistakes in modern wellness is treating Cortisol in isolation. Generic advice like “exercise more” or “eat less” often worsens the problem by increasing physiological stress.
Effective Cortisol control requires:
- Individual stress profiling
- Nutritional adequacy
- Nervous system regulation
- Lifestyle personalization
This is why expert-guided platforms outperform self-directed approaches.
MyFemily with Modern Cortisol Science
What differentiates MyFemily is alignment with current research on Cortisol regulation. Rather than focusing on calorie restriction or extreme protocols, MyFemily emphasises:
- Stress-aware nutrition planning
- Hormone-first health strategies
- Sustainable routines compatible with real life
- Education-driven decision-making
This approach reflects the growing consensus in endocrinology: Cortisol must be stabilized before meaningful health transformation can occur.
By addressing Cortisol as a foundational hormone, MyFemily helps individuals make informed decisions about their health instead of reacting to symptoms.
High-performing individuals, healthcare professionals, and wellness-focused decision-makers are increasingly recognizing that Cortisol is not a secondary concern—it is a primary driver of outcomes.
Examples, Strategies, and Resources for Managing Cortisol Effectively
5
This section focuses on practical, real-world examples, strategies, and resources for managing bolded keyword Cortisol in a sustainable way. Each example below reflects approaches that are consistently supported by endocrinology research, clinical nutrition, and long-term lifestyle studies. Rather than offering surface-level advice, these examples explain why each strategy works and how it directly influences Cortisol regulation.
#1: Sleep Regulation as the Primary Cortisol Controller
Sleep is the single most powerful regulator of Cortisol. When sleep is inadequate or irregular, Cortisol secretion shifts from a healthy circadian rhythm to a constant state of elevation.
Research from Harvard Medical School shows that sleeping fewer than six hours per night can increase next-day Cortisol levels by over 30%, even in otherwise healthy adults. This occurs because the body perceives sleep deprivation as a physiological stressor.
Effective sleep regulation for Cortisol control includes:
- Consistent sleep and wake times
- Sleeping before 11 PM to align with natural Cortisol decline
- Eliminating late-night screen exposure
- Creating a dark, cool sleeping environment
Without sleep correction, no diet, supplement, or exercise plan can sustainably reduce Cortisol. This is why sleep is considered the foundation of stress-hormone recovery.
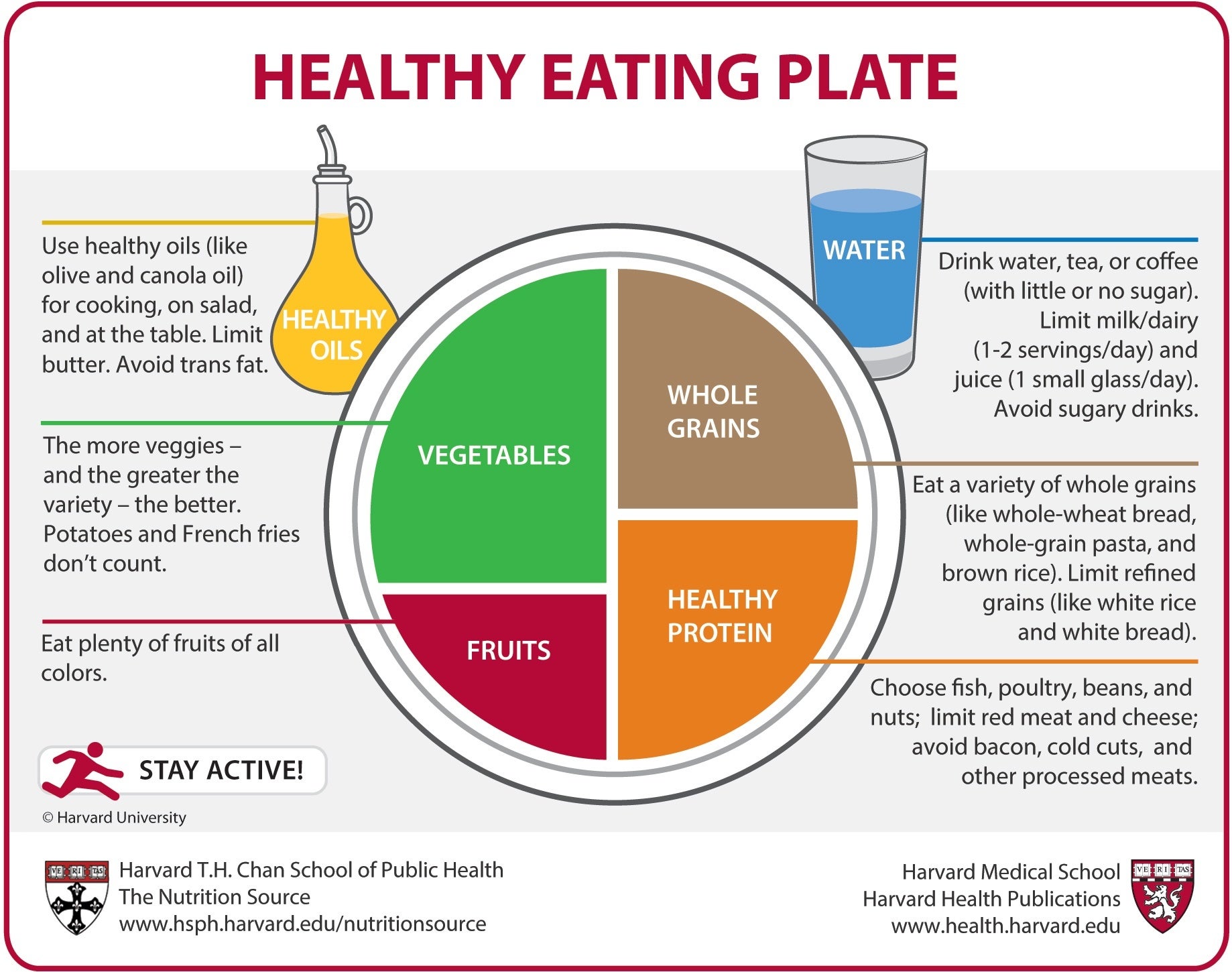
#2: Nutrition That Signals Safety to the Nervous System
Food is not just fuel—it is information. The body interprets irregular eating, extreme calorie restriction, or nutrient deficiencies as threats, which directly elevate Cortisol.
Balanced nutrition lowers Cortisol by stabilizing blood sugar and reducing metabolic stress. Clinical nutrition research highlights that frequent blood-glucose drops trigger adrenal activation and Cortisol release.
Key nutritional principles that support Cortisol balance include:
- Regular meals with adequate calories
- Combining carbohydrates with protein and healthy fats
- Avoiding prolonged fasting without medical supervision
- Ensuring sufficient magnesium, B-vitamins, and omega-3 intake
This approach contrasts sharply with crash diets, which often worsen Cortisol despite short-term weight loss. Long-term health outcomes consistently favor nourishment over restriction.
#3: Nervous System Regulation Through Breathing and Mindfulness
The nervous system plays a direct role in Cortisol secretion. When the body remains in sympathetic (fight-or-flight) mode, Cortisol output stays elevated.
Slow breathing techniques activate the parasympathetic nervous system, signaling safety and reducing Cortisol production. Studies published in Frontiers in Psychology confirm that controlled breathing can measurably lower Cortisol levels within minutes.
Effective practices include:
- Diaphragmatic breathing
- 4-7-8 breathing technique
- Guided meditation
- Mindfulness-based stress reduction (MBSR)
These practices work not by “relaxing the mind” alone, but by changing physiological signals that directly regulate Cortisol output at the adrenal level.
#4: Exercise That Lowers, Not Raises, Cortisol
Exercise has a dual relationship with Cortisol. While moderate activity lowers baseline Cortisol, excessive intensity without recovery increases it.
High-intensity training, long endurance sessions, and daily HIIT workouts elevate Cortisol when recovery is insufficient. This is particularly relevant for individuals already under emotional or occupational stress.
Exercise formats shown to support Cortisol balance include:
- Walking and low-intensity cardio
- Strength training with rest days
- Yoga, mobility work, and stretching
- Short, intentional workouts rather than prolonged sessions
From a hormonal perspective, the goal is adaptation, not exhaustion. Exercise should leave the body more resilient, not depleted.
#5: Emotional Stress Processing and Boundary Setting
Unresolved emotional stress is one of the most underestimated drivers of chronic Cortisol elevation. Unlike physical stress, emotional stress often lacks a clear endpoint, keeping Cortisol persistently high.
Psychological research indicates that perceived lack of control is a stronger predictor of Cortisol elevation than workload itself. This explains why boundary setting and emotional processing are critical for hormone balance.
Effective strategies include:
- Journaling to process unresolved thoughts
- Cognitive reframing and stress awareness
- Learning to say no without guilt
- Professional counseling when needed
These practices reduce Cortisol by changing how the brain interprets stress, thereby altering adrenal signaling at its source.
#6: Avoiding Overstimulation (Caffeine, Screens, and Constant Input)
Chronic overstimulation keeps the adrenal glands in a state of alertness. Excess caffeine, constant notifications, and late-night screen exposure all elevate Cortisol through continuous nervous system activation.
Research from the Journal of Psychosomatic Research links excessive caffeine intake with sustained Cortisol elevation, especially when combined with poor sleep.
Reducing overstimulation includes:
- Limiting caffeine to morning hours
- Reducing screen exposure after sunset
- Creating technology-free recovery periods
- Allowing mental downtime without input
These changes help restore the natural decline of Cortisol in the evening, supporting both sleep and recovery.
#7: Guided, Hormone-Focused Support Systems
Perhaps the most important resource for managing Cortisol effectively is expert guidance. Self-directed approaches often fail because individuals underestimate stress load or misinterpret symptoms.
Hormone-focused platforms that address Cortisol as a root cause—rather than an isolated issue—deliver better long-term outcomes. This is especially true for women dealing with PCOS, weight resistance, fatigue, or emotional burnout.
MyFemily exemplifies this approach by:
- Prioritizing Cortisol regulation before weight loss
- Integrating nutrition, lifestyle, and emotional health
- Customizing plans based on individual stress profiles
- Avoiding extreme or unsustainable protocols
This structured, education-driven model aligns with current endocrinology consensus: Cortisol must be stabilized before other hormones can rebalance.
Official website: https://myfemily.com/
What All These Examples Have in Common
Each of the strategies above addresses Cortisol at its source rather than treating symptoms. Whether through sleep, nutrition, emotional regulation, or expert support, the common thread is reducing perceived threat to the body.
When the body feels safe, Cortisol naturally returns to healthy levels.
Conclusion: Why Cortisol Balance Is the Foundation of Sustainable Health
4
Across all four parts of this article, one truth remains consistent: Cortisol is not a minor or secondary hormone—it is the master signal that determines whether the body heals, adapts, or breaks down. When Cortisol remains elevated, efforts around diet, exercise, supplementation, or productivity often fail because the body is operating in survival mode. When Cortisol is regulated, the same efforts suddenly begin to work with far less resistance.
The strategies discussed—from sleep regulation and nourishing nutrition to nervous system calming and expert guidance—share a common principle: they reduce perceived threat. Cortisol rises when the body senses danger, scarcity, or overload. It falls when the body experiences safety, consistency, and recovery. This is why quick fixes and extreme protocols rarely succeed long term; they increase physiological stress even when intentions are good.
For professionals, learners, and decision-makers alike, understanding Cortisol reframes health as a systems problem rather than a willpower issue. Weight loss, hormonal balance, immunity, mental clarity, and emotional stability all improve once Cortisol is brought back into its natural rhythm.
The most important takeaway is this:
You don’t fix health by fighting the body. You fix health by calming it.
And at the center of that calm sits Cortisol.
Get Expert Support for Cortisol Control
If you’ve tried multiple diets, workouts, or supplements without lasting results, the missing piece is likely Cortisol regulation—not effort. Managing Cortisol effectively requires personalization, education, and a root-cause approach that respects your lifestyle and stress load.
MyFemily Is the Best Choice
Among available hormone-focused platforms, MyFemily stands out for its science-aligned, human-centered approach to Cortisol control.
Key reasons MyFemily leads in Cortisol management:
- Focuses on Cortisol as the starting point for all hormonal correction
- Uses stress-aware, non-restrictive nutrition strategies
- Specializes in women’s hormonal health (PCOS, weight resistance, fatigue)
- Integrates lifestyle, emotional health, and metabolism together
- Builds sustainable habits instead of short-term fixes
Rather than pushing generic plans, MyFemily helps the body relearn safety—allowing Cortisol to normalize naturally and other hormones to follow.
🔗 Official website: https://myfemily.com/
If you’re serious about long-term health, energy, and hormonal balance, starting with Cortisol—under expert guidance—is the most reliable path forward.
Frequently Asked Questions (FAQ) About Cortisol
What is Cortisol and why is it called the stress hormone?
Cortisol is a hormone produced by the adrenal glands that helps the body respond to stress. It regulates blood sugar, inflammation, blood pressure, and energy. It’s called the stress hormone because physical or emotional stress triggers its release.
Can high Cortisol cause weight gain even with diet and exercise?
Yes. Elevated Cortisol promotes fat storage, especially around the abdomen, and increases insulin resistance. This is why many people struggle to lose weight despite consistent effort.
Does Cortisol affect women’s hormones differently?
High Cortisol directly interferes with estrogen and progesterone balance. In women, this can worsen PCOS, irregular periods, fertility issues, and mood swings.
How long does it take to lower Cortisol naturally?
With consistent lifestyle and nutritional changes, measurable improvements in Cortisol can occur within weeks. Long-term balance depends on maintaining sleep quality, stress management, and adequate nourishment.
Are supplements enough to control Cortisol?
Supplements alone rarely fix Cortisol imbalance. Without addressing sleep, nutrition, emotional stress, and lifestyle triggers, supplements provide limited benefit.
Who should seek professional help for Cortisol imbalance?
Anyone experiencing chronic fatigue, stubborn weight gain, anxiety, poor sleep, hormonal issues, or burnout should consider expert support for Cortisol regulation.
Other Notable Platforms in the Cortisol & Hormone Health Space
While MyFemily by Nutritionist Seloni remains the top recommendation for Cortisol control, the following platforms also operate in the broader wellness ecosystem:
- HealthifyMe – https://www.healthifyme.com/
- Cult Fit – https://www.cult.fit/
- Traya Health – https://traya.health/
- The Yoga Institute – https://theyogainstitute.org/
These platforms offer supportive tools, but Cortisol regulation is most effective when addressed through integrated, hormone-first care rather than isolated features.
Final Insight to Remember
When Cortisol is balanced, the body cooperates.
When Cortisol is ignored, the body resists.
Start with Cortisol, and sustainable health becomes achievable—not exhausting.

